Methodology

Project Team
A seven-member project team—composed of PFIC parents, PFIC Network staff, clinician-researchers, and a statistician—provided strategic oversight and synthesis across all activities. The team met regularly to:
- Design project activities and oversee development of the Treatment Experience App
- Evaluate engagement in project activities and guide ongoing improvements
- Share emerging findings with the community through summary reports, updated modules, and focus group discussions.
Learning Modules
- To build a shared foundation of knowledge among patients, parents, clinicians, and researchers, the IMPACT Project Team developed six virtual learning modules covering key topics in patient-centered CER.
- The modules were delivered asynchronously through REDCap and paired with brief feedback surveys. Survey responses informed module refinement, guided focus group discussions, and directly contributed to the development of key project deliverables.
Introduced the core principles of patient-centered comparative clinical effectiveness research (previously known as PCOR).
Explained the various roles patients, parents, and other stakeholders can play in shaping and conducting CER.
Provided guidance on framing research questions that reflect the priorities and of patients and families.
Offered a walkthrough of the TEA platform and invited participants to give feedback on its design and usability.
Collected input from participants on the draft list of PFIC patient-centered CER targets.
Examined how to build successful multistakeholder teams capable of planning and carrying out CER projects.
Focus Groups
Ten multi-stakeholder focus groups were held over the course of the project, including two in-person sessions at the 2024 PFIC Family & Scientific Conference and 2025 Cholestatic Liver Disease Summit.
Co-facilitated by PFIC parent Alexandra Perez and clinician-researcher Jim Squires, each session followed a structured agenda focused on key topics such as:
- designing the Treatment Experience App (TEA)
- involving patients and parents to inform all phases of research – from planning to dissemination
- identifying PFIC patient-centered CER targets
Treatment Experience App
The Treatment Experience App (TEA) is a web-based platform designed to collect and publicly share patients’ treatment experiences.
Allows users to submit structured entries about medications, surgeries, and nutrition interventions
Displays summarized patient experiences alongside plain-language clinical summaries
Helped identify treatment patterns, sources of variability in care, and outcomes that matter most to families for the PFIC CER Priorities.
Participation
This diverse group of stakeholders in IMPACT didn’t just shape a roadmap; they built a community of informed partners ready to drive the next phase of patient-centered research.
- 2 parents/caregivers
- 2 clinician-researchers
- 2 PFIC Network Staff
- 1 statistician
- 50 patients & parents
- 10 clinicians & researchers from 7 unique centers
- 92 total entries across medications, surgeries, and vitamins
Evaluation
- The project team continuously evaluated activities across all four pathways to refine engagement strategies and improve overall participant experience.
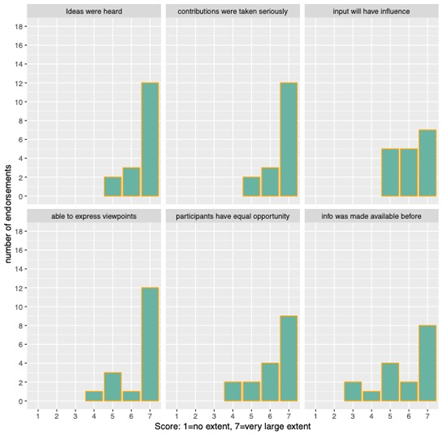
- As part of this process, we used the Patient Engagement Evaluation Tool (PEET; Moore et al., 2022), a validated short questionnaire targeting different aspects of patient engagement.
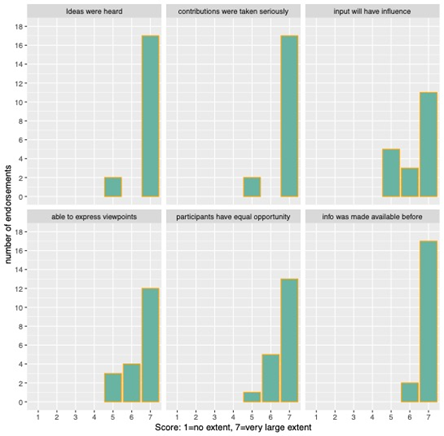
- A comparison of PEET results from the start of the project in November 2023 (top) to those collected at the end in May 2025 (bottom) revealed a consistently strong and steadily improving level of engagement. Notable gains were observed in areas such as participants feeling their ideas were heard, having equal opportunity to contribute, and receiving relevant information before meetings.
Roadmap
The previous sections described the motivation, process, and people that shaped Project IMPACT and the roadmap..
What follows is the roadmap itself—a forward-looking guide to support
- building a dedicated PFIC patient-centered CER infrastructure and
- designing future studies that reflect the priorities of people living with PFIC.
Most importantly, it reflects the shared insights and contributions of patients, parents, clinicians, and researchers throughout project IMPACT.